The ACTION Study
The ACTION (Awareness, Care and Treatment In Obesity MaNagement) Study is the first multidisciplinary study to explore the barriers and perspectives in the sphere of obesity care.
ABOUT THE STUDY
Overview
Learn how the results of the ACTION Study can shift the way you see and treat obesity
ACTION Study explores attitude and behaviors about obesity
Obesity is recognized by leading health organizations, including the American Medical Association and the World Health Organization, as a chronic disease.1-5 Associated with decreased life expectancy and many comorbidities, obesity requires a long-term and comprehensive management approach to help people with the disease achieve and maintain successful weight loss.6,7
However, many people with obesity do not receive optimal medical care and support, often due to multiple barriers that have been identified in prior research.8,9
The ACTION Study is the first to explore these barriers and perspectives on obesity among three important groups in the sphere of obesity care: people with obesity, health care professionals, and employers. Each of these groups plays an important role in the care and support of people with obesity.
Three phases of the ACTION Study10

References:
1. American Medical Association House of Delegates. Recognition of obesity as a disease. Resolution 420 (A-13). Accessed October 17, 2016. http://www.npr.org/documents/2013/jun/ama-resolution-obesity.pdf
2. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1-253.
3. Bray GA, Kim KK, Wilding JPH; World Obesity Federation. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715-723.
4. Mechanick JI, Garber AJ, Handelsman Y, Garvey WT. American Association of Clinical Endocrinologists’ position statement on obesity and obesity medicine. Endocr Pract. 2012;18(5):642-648.
5. McKinney L. Diagnosis and Management of Obesity. American Academy of Family Physicians (AAFP). Accessed December 20, 2017. https://www.aafp.org/dam/AAFP/documents/patient_care/fitness/obesity-diagnosis-management.pdf
6. Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25ptB):2985-3023.
7. Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
8. Puhl RM, Huer CA. Obesity stigma: important considerations for public health. Am J Pub Health. 2010;100(6)1019-1028.
9. Ruelaz AR, Diefenbach P, Simon B, Lando A, Arterburn D, Shekelle PG. Perceived barriers to weight management in primary care—perspectives of patients and providers. Gen Intern Med. 2007;22:518-522.
10. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26(1):61-69.
ABOUT THE STUDY
Study methodology
ACTION Study objectives
1
Create a better understanding of the barriers that prevent people with obesity from receiving the medical care and support needed to improve health
2
Generate insights to guide collaborative action to improve care, education, and support for people with obesity
3
Create a platform for communication to help change how people with obesity, health care professionals, and employers manage, treat, and support obesity
To achieve these objectives, the ACTION Study involved a comprehensive literature review, qualitative research, and quantitative surveys of more than 3,000 people with obesity, 600 health care professionals, and 150 employers in the United States. In all, this research produced data points around the perceptions of obesity, the care people with obesity receive, and the support and resources that HCPs and employers offer to people with obesity.
The ACTION Study is sponsored by Novo Nordisk.
Qualitative research design
To begin to identify perspectives on obesity and inform the design of the quantitative survey, focus groups and interviews were conducted with 43 people with obesity and 24 health care professionals (12 primary care physicians and 12 weight-loss specialists).1

Six focus groups for people with obesity were held in New York City, Dallas, and San Francisco. Participants were above 18 years old and met the criteria for obesity diagnosis. Groups were divided by gender and obesity class (I, II or III).1

Telephone interviews with primary care providers and obesity specialists (physicians and nurse practitioners) were conducted to explore perceptions of obesity treatments, patient interactions, and observations of patient weight-loss experiences. Obesity specialists were certified by the American Board of Obesity Medicine.1
For both groups, participants were identified by independent sources.
Quantitative research results
Based on the qualitative research findings, an extensive quantitative survey was conducted with people with obesity, health care professionals, and employers. Study results reveal key barriers to obesity care, including differing attitudes, perceptions, and behaviors that may lead to a lack of collaboration and action.
The quantitative data was collected from and reflects the perspectives of these three groups:

Reference:
1. Kaplan L, Golden A, O'Neil P, et al. Divergence of patient and clinician perceptions of obesity and weight management. Poster presented at: ObesityWeek 2015; November 2-6, 2015; Los Angeles, CA.
ABOUT THE STUDY
Qualitative research
ACTION Study qualitative research indicates differences in perception about obesity among participants1
People with obesity and health care professionals diverge on cause of obesity and impact on health.
The qualitative research findings from the ACTION Study highlight several key differences in perceptions between people with obesity and health care professionals, particularly around the understanding of the impact of obesity on health, as well as barriers to weight loss. The qualitative research informed the design of more extensive quantitative research.
Reference:
1. Kaplan L, Golden A, O'Neil P, et al. Divergence of patient and clinician perceptions of obesity and weight management. Poster presented at: ObesityWeek 2015; November 2-6, 2015; Los Angeles, CA.
ABOUT THE STUDY
Quantitative research
ACTION Study reveals key barriers to effective obesity care1
The first US nationwide study to investigate barriers to obesity management from the perspective of people with obesity, health care professionals, and employers, the ACTION Study quantitative research follows a literature review and robust qualitative research. The data were collected through surveys of more than 3,000 people with obesity, 600 health care professionals, and 150 employers.
Despite agreement among people with obesity, health care professionals, and employers that obesity is a disease, the ACTION Study reveals significant differences among the participant groups that provide insight to the key barriers that may prevent people with obesity from accessing medical care to effectively manage their weight.1
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Overview
ACTION Study finds few people with obesity seek and receive long-term obesity care1
Despite changing attitudes towards obesity and its increasing recognition as a chronic, serious, and progressive disease, many barriers to effective care remain. These barriers are reflected in the insufficient interaction between patients and health care professionals relating to dialogue and treatment of obesity.
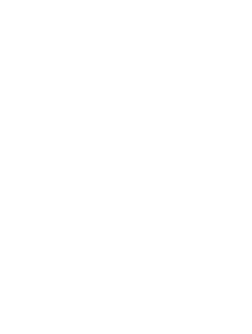
Conversations about weight are insufficient1

ACTION Study identifies five key barriers to obesity care1
The ACTION Study explored attitudes, perceptions, and behaviors among all 3 groups that are preventing effective and comprehensive obesity care.

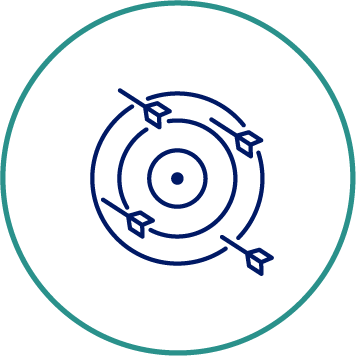
1. Weight-loss challenges
People with obesity engage in several serious weight-loss attempts, but few are able to maintain the achieved weight loss

2. Reluctance to seek help
Despite recognition of obesity as a disease, most people with obesity consider weight loss to be completely their own responsibility, which may prevent them from seeking help from their health care professional

3. Inadequate diagnosis
Many people with obesity have not received a formal diagnosis of obesity

4. Inadequate follow-up
The patient-provider dialogue about weight management is insufficient with few follow-up visits
5. Unclear wellness offerings
Employer wellness programs are not meeting the needs of people with obesity
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Weight-loss challenges
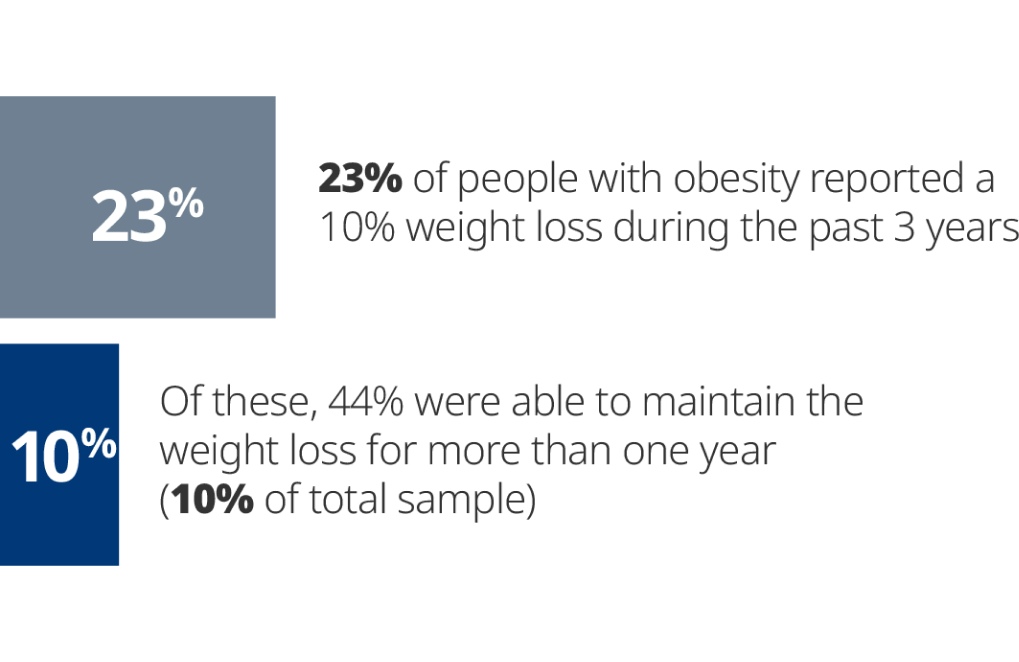
People with obesity engage in several serious weight loss attempts, but only a few are able to maintain the achieved weight loss.1
People with obesity reported many serious weight-loss attempts, but those who achieved weight loss had difficulty maintaining it
Weight-loss goals
People with obesity (84%) and health care professionals (88%) agree that a 10% weight loss would be beneficial to overall health, a statistic that aligns with scientific literature that states a 5% to 10% weight loss can help improve some obesity-related diseases.1-9
However, the average weight-loss goal set between people with obesity and their health care professional is reported as 20% weight loss.1

The bottom line:
Weight-loss challenges
Losing weight and maintaining weight loss is difficult, but people with obesity make multiple serious attempts to lose weight.
References
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
2. Jensen MD, Ryan DH, Apovian CM, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25ptB):2985-3023.
3. Knowler WC, Barrett-Connor E, Fowler SE, et al; for the Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6)393-403.
4. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481-1486.
5. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56(2):320-328.
6. Tuomilehto H, Seppä J, Uusitupa M, et al. The impact of weight reduction in the prevention of the progression of obstructive sleep apnea: an explanatory analysis of a 5-year observational follow-up trial. Sleep Med. 2014;15(3):329-335.
7. Foster GD, Borradaile KE, Sanders MH, et al; for the Sleep AHEAD Research Group of the Look AHEAD Research Group. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169(17):1619-1626.
8. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep. 2013;36:641-649.
9. Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr Obes Rep. 2017;6(2):187-194.
BARRIERS TO CARE
Reluctance to seek help
Most people with obesity and health care professionals believe obesity is a disease, and many patients with obesity view it as serious, or more serious, than many other health conditions, including high blood pressure, diabetes, and depression.
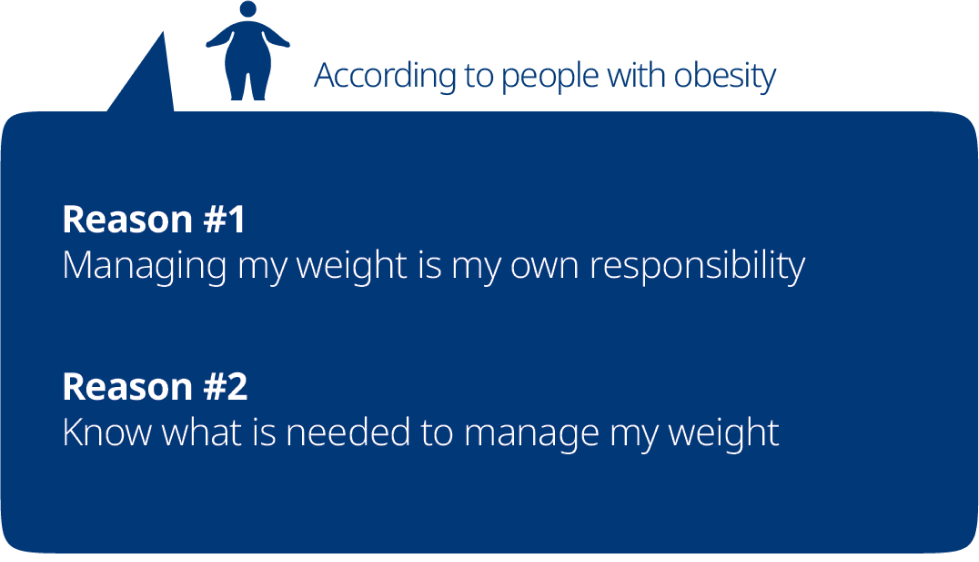
Most people with obesity view weight loss as solely their responsibility, which may prevent them from seeking help1

Views on personal responsibility for weight loss1
Even though people with obesity consider obesity a disease, most view weight loss to be completely their own responsibility. However, most health care professionals reported that they have a responsibility to actively contribute to their patients’ weight loss.

Differing perspectives: Top reasons why people with obesity don’t seek weight-loss help from their health care professional1

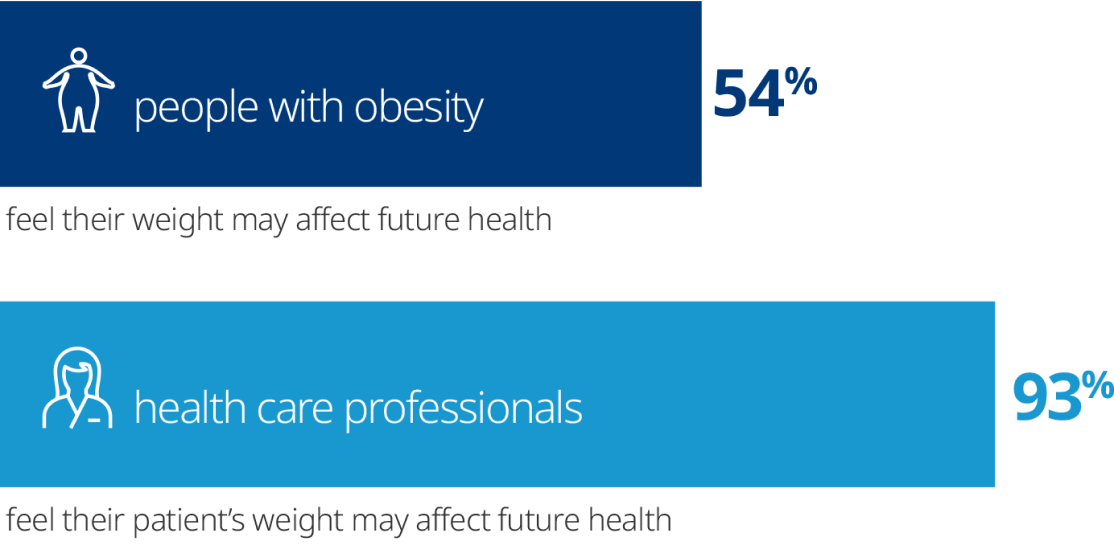
The impact of weight on future health1
People with obesity and health care professionals have different levels of concern when it comes to how a person’s weight affects future health.
The bottom line:
Reluctance to seek help
Despite general consensus that obesity is a disease, there is a strong belief held by people with obesity that weight loss is their own responsibility. This may contribute to their not seeking medical care for their disease.
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Lack of diagnosis
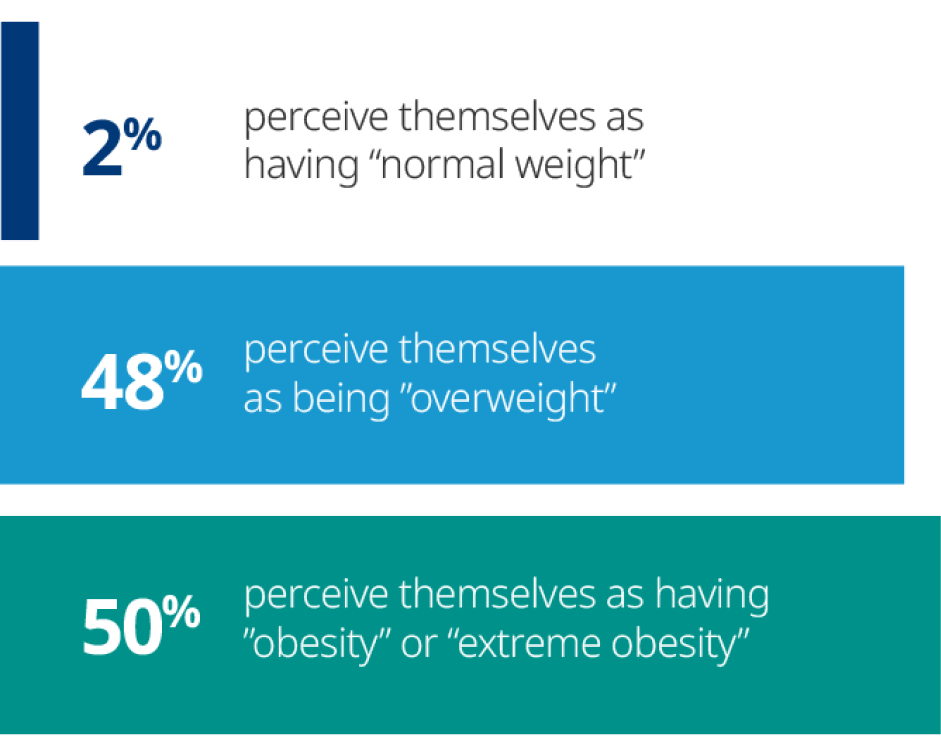
Although all ACTION Study participants actually had obesity based on self-reported height and weight, only slightly more than half reported having received a formal diagnosis of the disease. When it comes to self-perception, about half considered themselves as being overweight while the other half considered themselves as having obesity.
Many people with obesity have not received a formal diagnosis of obesity1

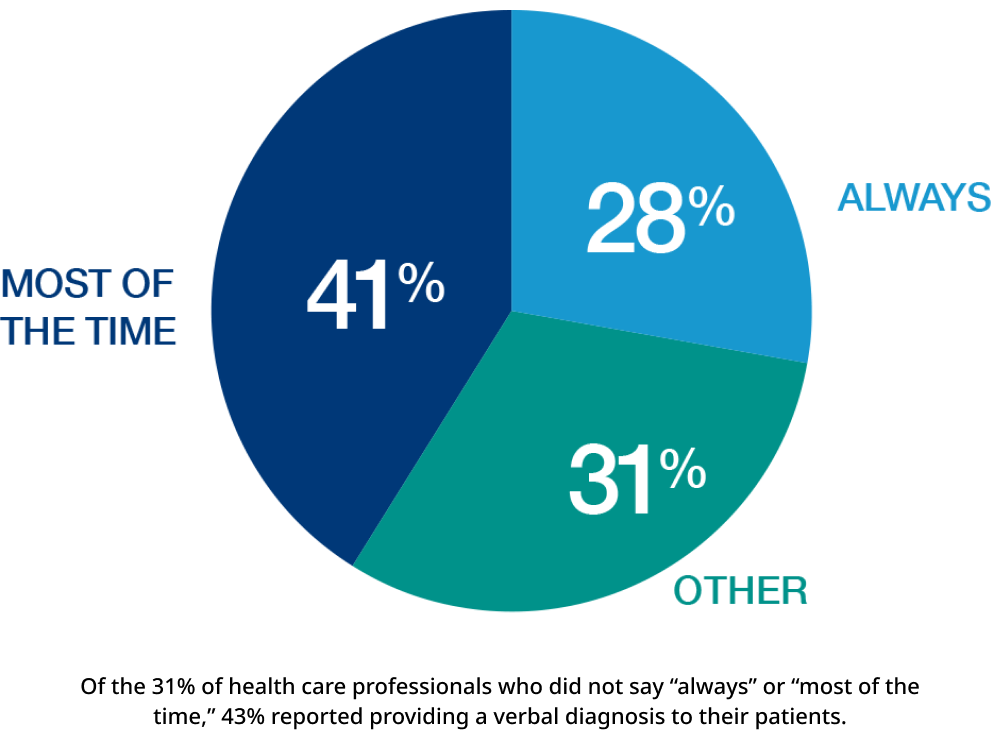
Health care professionals inconsistently record diagnosis of obesity1
The majority of health care professionals reported that they record “overweight” or “obesity” in the medical record.
Bottom line: Lack of diagnosis
The first step to addressing a disease is recognizing and diagnosing it. Thus, the lack of formal obesity diagnoses is a barrier to obesity management.
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Inadequate follow-up
The majority of people with obesity say they have spoken with a health care professional about their weight within the past 5 years, but only slightly more than a third say they have discussed a weight-loss plan with their health care professional within the past 6 months.
The patient-provider dialogue about weight management is insufficient with few follow-up visits1
Differing perceptions around initiation of obesity dialogue
Both people with obesity and health care professionals reported initiating these conversations. About half (47%) of people with obesity say they initiate the conversation, while two-thirds (67%) of health care professionals say they initiate the weight-management dialogue.
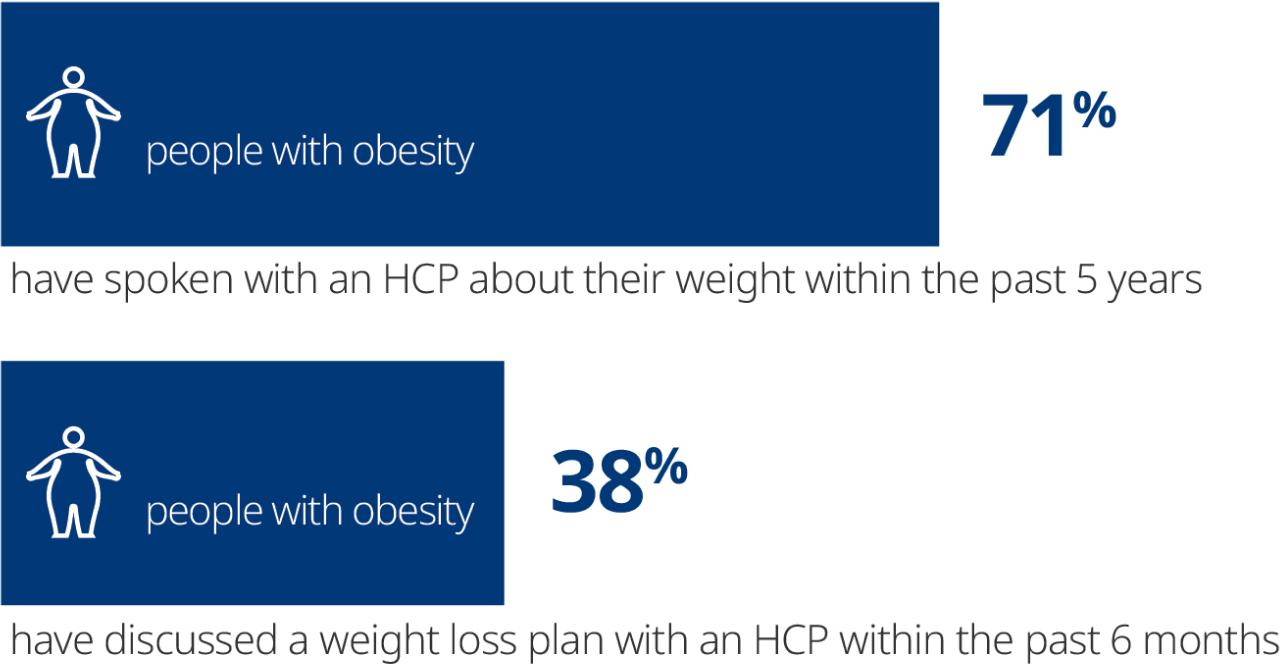
Many health care professionals are comfortable discussing weight1
Most health care professionals (67%) say they are very or extremely comfortable discussing weight management with their patients, but they cite hurdles to initiating these conversations.
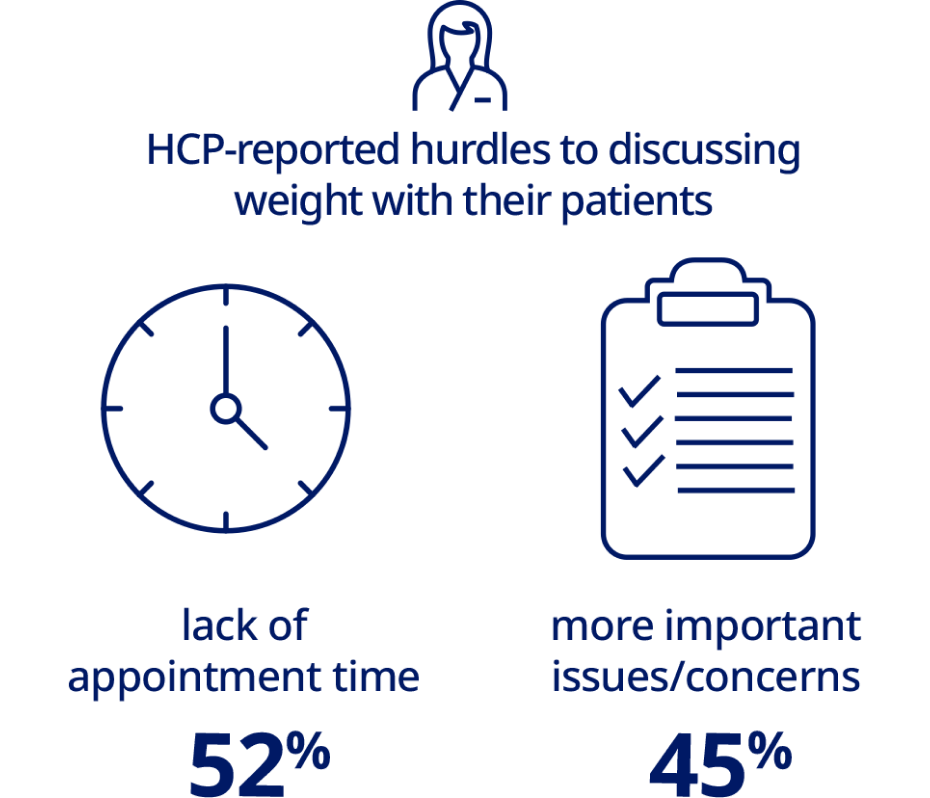
Limited follow-up appointments1
Among people with obesity who discussed their weight with a health care professional, only 24% reported that a weight-related follow-up appointment was scheduled. More than 95% of people with obesity have kept or intended to keep the follow-up appointment.

Learn how people with obesity can initiate the weight-management conversation with health care professionals
The bottom line:
Inadequate follow-up
Insufficient dialogue about weight management and lack of follow-up appointments present a key barrier to chronic care of obesity.
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Unclear wellness offerings
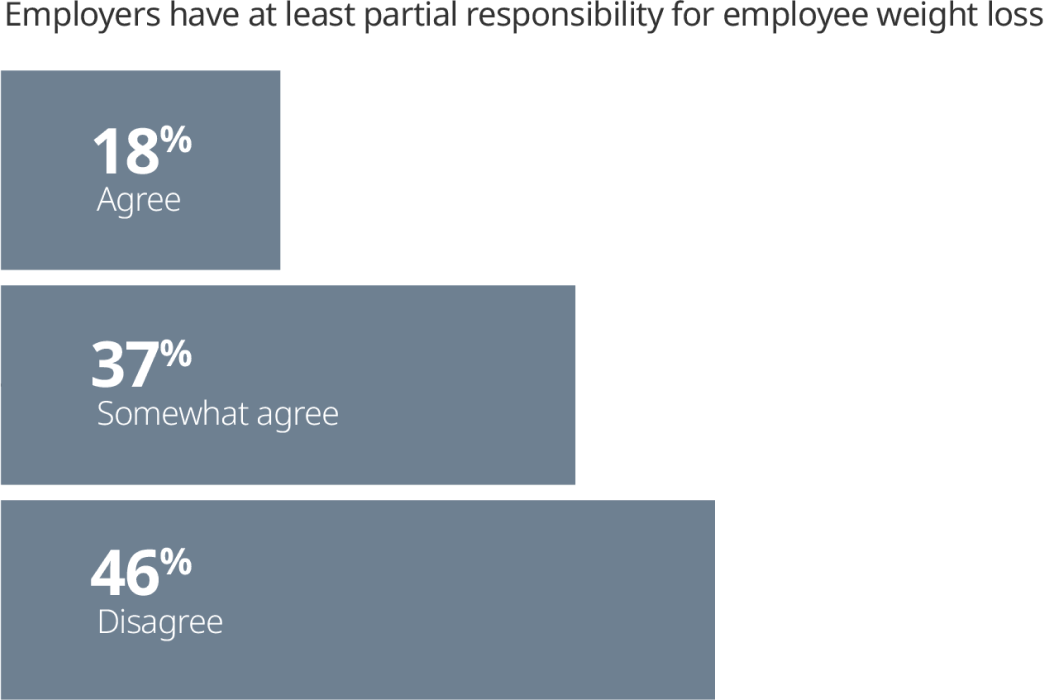
Like people with obesity and health care professionals, the majority of employers (64%) agree that obesity is a disease; however, fewer employers agree they have at least partial responsibility for employees’ weight loss.
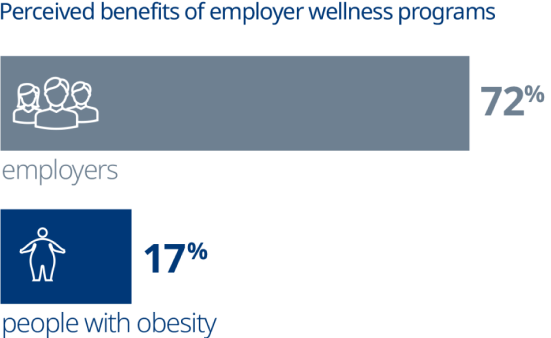
At the same time, employers are motivated to offer wellness programs and more than three quarters (77%) of employers reported providing health and wellness information to employees. Some of these programs include weight-management components.
Employer wellness programs are not meeting the needs of people with obesity1
Employers offer wellness programs for a variety of reasons1

75%
Reduce insurance premiums/claims

72%
Promote healthy behaviors among employees

70%
Improve the physical well-being of employees

61%
Support the well-being of employees and their families

53%
Improve work productivity
Value in wellness programs perceived differently by employers and people with obesity1
The wellness programs offered by employers are not perceived by the majority of people with obesity as helpful.
Insurance coverage for medical treatment of obesity is a source of concern for employers1
A small number of people with obesity (13%) reported that their employer offers insurance coverage for the medical treatment of obesity. Employers cited multiple reasons for their concern around coverage.




Learn about the impact of obesity in the workplace and how chronic weight-management initiatives can be implemented
The bottom line:
Unclear wellness offerings
Varying perceptions of the value of wellness programs, as well as employer concerns regarding insurance coverage, present a barrier to effective obesity management.
Reference:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
BARRIERS TO CARE
Take ACTION
Although obesity is generally perceived to be a disease, it is not consistently being treated as such1

There is a strong belief held by people with obesity that weight loss is their own responsibility. This may contribute to a reluctance to seek medical care for their disease.

Health care professionals feel a responsibility to support their patients' weight-management efforts, but they don't always offer an obesity diagnosis. Conversations with their patients are not always followed up in subsequent appointments.

While employers have the desire to improve the physical well-being of employees, their offerings are not effectively supporting the weight-loss efforts of people with obesity.
Collaborative efforts are necessary for more effective obesity care
The barriers identified in the ACTION Study highlight the need for collaborative efforts that can lead to better understanding of obesity and more effective solutions for obesity care.

Educate people with obesity, health care professionals, and employers about the biology, chronicity, and overall health impact of the disease. This could foster a greater willingness for these groups to work together to support weight management.
Learn more about obesity and the impact on the body.

Inform health care professionals about reasons why people with obesity may not discuss weight. This could reduce the reluctance among health care professionals to proactively initiate these important conversations.
Learn how health care professionals can best engage in productive weight management conversations with people with obesity.

Encourage health care professionals to regularly schedule follow-up visits focusing on the obesity diagnosis and the value of 5% to 10% weight loss, given patients’ inclination to keep these appointments.2-8 Such efforts will provide greater consistency and support to people with obesity, and underscore that obesity is a disease that requires chronic weight management.
Learn how health care professionals can deliver the message that weight loss as little as 5% can benefit patients.

Increase understanding among employers that obesity can be effectively treated as a disease, potentially helping them better promote wellness programs and more rigorously assess their effectiveness in line with the needs of people with obesity.
References:
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61-69.
2. Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25ptB):2985-3023.
3. Knowler WC, Barrett-Connor E, Fowler SE, et al; for the Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6)393-403.
4. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481-1486.
5. Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56(2):320-328.
6. Tuomilehto H, Seppä J, Uusitupa M, et al. The impact of weight reduction in the prevention of the progression of obstructive sleep apnea: an explanatory analysis of a 5-year observational follow-up trial. Sleep Med. 2014;15(3):329-335.
7. Foster GD, Borradaile KE, Sanders MH, et al; for the Sleep AHEAD Research Group of the Look AHEAD Research Group. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169(17):1619-1626.
8. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep. 2013;36:641-649.
RESOURCES
Organizations
Many credible organizations provide information and education on the latest scientific findings in obesity, as well as provide helpful resources on obesity management.
FOR PEOPLE WITH OBESITY
FOR HEALTH CARE PROFESSIONALS
Academy of Nutrition and Dietetics (AND)
American Academy of Physician Assistants (AAPA)
American Association of Clinical Endocrinologists (AACE)
American Association of Nurse Practitioners (AANP)
American Board of Obesity Medicine (ABOM)
American Congress of Obstetricians and Gynecologists (ACOG)
American Society for Metabolic and Bariatric Surgery (ASMBS)
FOR EMPLOYERS
FOR POLICYMAKERS
The obesity-related websites on this page are independently operated and not managed by Novo Nordisk. Novo Nordisk assumes no responsibility for any information provided through these sites.

ADVOCACY AND RESOURCES
Check out some frequently asked questions about obesity

INITIATING A PLAN
Pharmacotherapy may help patients keep weight off